The District likes to boast that affordable health insurance is available to any resident, but one group has struggled to get access to health care in recent years. DC residents in the Healthcare Alliance program face barriers to eligibility like no other public program in the District. If the District really is to be a place where health insurance is universally accessible, we must make it easier for eligible residents to apply for and maintain their Alliance benefit.
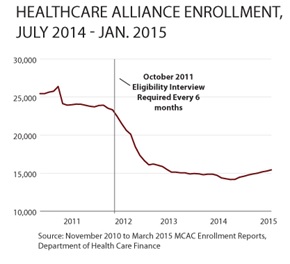
The Healthcare Alliance program serves low-income residents who are not eligible for Medicaid, Medicare, or subsidies on DC Health Link — mostly undocumented immigrants. In 2011, DC implemented a strict eligibility rule which requires Alliance beneficiaries to have an in-person, face-to-face interview with the Department of Human Services (DHS) every six months. This is one of the strictest eligibility requirements for public programs in DC, and has led to the program shrinking from 25,000 beneficiaries to 15,000 beneficiaries. That likely means thousands of eligible residents are going without insurance.
There are several problems with the requirement:
- It is hard for eligible beneficiaries — especially those who work and/or have young children — to maintain their benefit. The frequency of the requirement leads to a large volume of people coming into public benefit service centers where the interviews take place. Alliance beneficiaries must often make multiple trips because the service center has reached capacity and can’t see them, a lack of available language assistance, long lines, submitted paperwork that ends up lost or not accounted for, and delays in processing information. The Department of Healthcare Finance reports that between 50 and 67 percent of cases are terminated because of failure to complete the interview requirement. This leaves many without health coverage.
- It costs DC money. DC has to hire more staff to manage the increased volume that come into the service centers. What’s more, the requirement appears to have a direct impact on higher health costs for the program, as many residents avoid primary care and only sign up for the Alliance when they are medically very needy.
- It is operationally troublesome for DHS. The Department of Human Services has long wait and processing times for public benefit programs, and the added volume of beneficiaries who must fulfill the interview requirement only adds to those problems. Alliance beneficiaries report lining up as early as 6 a.m. just to be seen by staff.
For these reasons, five community groups have drafted a letter in hopes of changing requirements of the DC Healthcare Alliance program. The letter proposes to:
- Change the 6-month interview requirement to an annual interview. This change would put the Alliance program’s rules more in line with Medicaid, and ease long lines and wait times at DC’s social service intake centers.
- Allow community health workers to assist with parts of the application and annual interview. This would alleviate some of DHS’s immediate workload pressures at service centers and help beneficiaries who have relationships with a health center.
For a copy of today’s blog, click here.
