Chairman Gray and members of the Committee, thank you for the opportunity to testify today. My name is Kate Coventry, and I am a senior policy analyst at the DC Fiscal Policy Institute. DCFPI is a nonprofit organization that promotes budget choices to reduce economic and racial inequality and build widespread prosperity in the District of Columbia through independent research and thoughtful policy recommendations.
My testimony focuses on the need for behavioral health services for residents with traumatic brain injuries (TBI), also known as acquired brain injuries. I ask the Department of Health Care Finance, the Deputy Mayor for Health and Humans Services, and the Committee on Health to work with advocates and providers to create a robust system of TBI screening and programming to meet this need. The most direct path to ensuring DC residents with co-occurring TBI and behavioral health conditions receive needed treatment would be to allow behavioral health service providers to bill for services rendered even when TBI is the primary diagnosis.
I will also testify about how the District should fund the Prescription Drug Monitoring Program Query and Omnibus Health Amendments Act of 2020, which will ensure that the DC Healthcare Alliance has low-barrier application and recertification requirements.
TBIs Have Significant Negative Effects
TBIs are injuries resulting from a blow or jolt to the head, or a penetrating injury to the head, that disrupts the function of the brain.[1] TBI in adults is associated with an increased risk for substance misuse, major depression, anxiety, and unemployment.[2]
TBIs can negatively affect self-regulation and executive functioning. Self-regulation refers to a person’s ability to manage behavior associated with stress and anxiety. For a person with a TBI, this might entail difficulty waiting or taking turns; difficulty calming down; or feeling overwhelmed in new places. Executive functioning refers to higher-order brain functions associated with setting goals, organizing, remembering, following directions, and focusing attention. People with TBIs can become easily confused or forgetful; have difficulty learning new information; filling out forms; and using public transportation. Some have difficulty problem-solving, and others have problems with judgment and decision-making. After experiencing a TBI, people may have trouble keeping track of time, making plans, making sure to complete plans or assignments, applying previously learned information to solve problems, analyzing ideas, and looking for help or more information when needed.
Vulnerable Populations are Particularly at Risk
TBIs can happen to anyone, but there are people who face a greater risk of acquiring a TBI. National statistics show that 50 to 80 percent of homeless individuals have sustained at least one brain injury prior to homelessness.[3] Research suggests that TBIs may be a risk factor for becoming homeless.[4] Homeless individuals are also at a higher risk of acquiring a TBI because they are more likely to be victimized by assault, experience trauma, and have substance use disorders that can cause falls.[5] In 2010, 199 DC homeless individuals were surveyed and nearly two-thirds had a TBI.[6]
A 2016 survey of 159 adult DC behavioral health clients found that approximately 50 percent had a history of TBIs.[7] Additionally, active duty military personnel are at very high risk. Domestic violence survivors are also at high risk because “the head and face are among the most common targets of intimate assaults.”[8] And finally, a TBI is a common co-occurring disorder among people who are diagnosed with a major mental illness and who have a history of substance misuse and criminal justice involvement.
DC Residents with TBIs are Not Getting the Services They Need, with Devastating Implications
DC behavioral health providers generally do not screen, identify, or treat the symptoms of TBIs because TBI is not an official billable diagnosis in DC’s behavioral health system, and there is no system to train mental health providers. Community-based providers cannot receive payment for services provided to treat TBIs, whether it is a standalone diagnosis or co-occurring disorder.
The lack of services has terrible implications for individuals with TBIs. Research has found that people with cognitive impairments like TBIs may be falsely considered non-compliant and then get expelled from programs because these impairments prevent them from fully participating in the services. Or they are banned from sites because of “disruptive behavior or failure to comply with prescribed treatments.”[9] To the untrained eye, problems with executive functioning can look like lack of motivation, laziness, disregard for others, and a reluctance to engage in social activities. Given that a 2010 survey of 12 DC homeless service providers found that only one provider had received any training on TBIs, it is likely that many homeless individuals with a TBI are being excluded from mainstream homeless services.[10]
DC Can Look to Other Jurisdictions for Effective Service Models
DC should allow providers to bill for screenings and a wide range of services. There are a number of other jurisdictions that have implemented effective services that DC could build upon:[11]
- Screening and accommodations in both healthcare and behavioral health settings. It is essential that DC create a system of TBI screening and provide accommodations at its medical and psychiatric intake sites, including hospital emergency departments, jails, drug treatment programs, in-patient psychiatric units, core service agencies, and the Comprehensive Psychiatric Emergency Program (CPEP).
- Day programs provide individualized skills training, cognitive rehabilitation, and work reentry. They provide the opportunity for participants to relearn life skills, such as how to interact in social settings, negotiate public transportation to get to appointments, or how to cook a simple meal.
- Case management assists the consumer to address basic needs, such as keeping appointments, developing a therapy and medication schedule, and accessing public benefits.
- Residential Programs with specially trained staff.
DCFPI urges the Department of Health Care Finance, the Deputy Mayor for Health and Human Services, and the Committee on Health to work with advocates and providers to create a robust system of TBI screening and programming.
The District Should Fund Legislation that Reduces Barriers to Alliance Enrollment and Recertification
I encourage the District to fund the Prescription Drug Monitoring Program Query and Omnibus Health Amendments Act of 2020 which will ensure that the DC Healthcare Alliance has low-barrier application and recertification requirements. The Alliance is a program that provides critical health care coverage to residents with low incomes who do not qualify for Medicaid, most of whom are immigrants. Healthcare is a human right and truly vital during the current COVID-19 pandemic. The District should be doing all it can to ensure that as many residents as possible have access to insurance and that access is as easy as possible. DC should do this by removing onerous recertification requirements in the Healthcare Alliance.
Given their shared purpose, the DC Healthcare Alliance and Medicaid program should have identical, low-barrier application and recertification requirements. But the DC Healthcare Alliance requires participants to recertify every 6 months and requires participants to do at least one recertification annually in person. Medicaid only requires annual recertification and allows participants to do so online. These barriers contribute to both poor health outcomes and unnecessarily high program costs.[12] We shouldn’t erect higher barriers just because a resident is undocumented—DC is a welcoming city, and our policies should reflect that value.
We thank the Council and this Committee for acting to reduce the in-person requirement to once per year. And we thank the administration for ensuring that no one loses eligibility during the public health crisis by temporarily waiving the in-person interview requirement for the Alliance, but we need permanent changes to Alliance application and recertification procedures to build a just recovery.
Shortened Eligibility Period Has Led to Turnover, Poorer Health, and Higher Costs
In 2011, DC implemented restrictive procedures residents had to follow to maintain their Alliance eligibility, including in-person interviews every six months, whereas Medicaid only requires annual recertification and no in-person interviews. The change in Alliance immediately led to a sharp drop in participation (Figure 1). Today, thousands of residents who should have health insurance do not, and the uninsured rate is much higher among Latinx DC residents[13] than others.
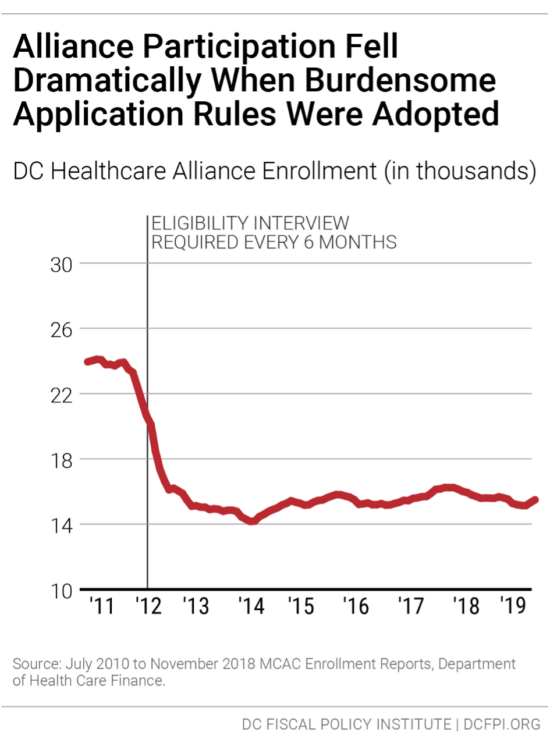
The restrictive rules also contribute to a high rate of turnover in the Alliance, as residents join the program but then drop off, due to the time-intensive requirements. Only 55 percent of Alliance participants renew their eligibility when it comes up, data from the District’s Department of Health Care Finance (DHCF) show.[14] Given that many Alliance members are working at jobs without paid leave and that visiting a Department of Human Services center can take an entire day or longer, it is not surprising that many are not able to renew their benefits.
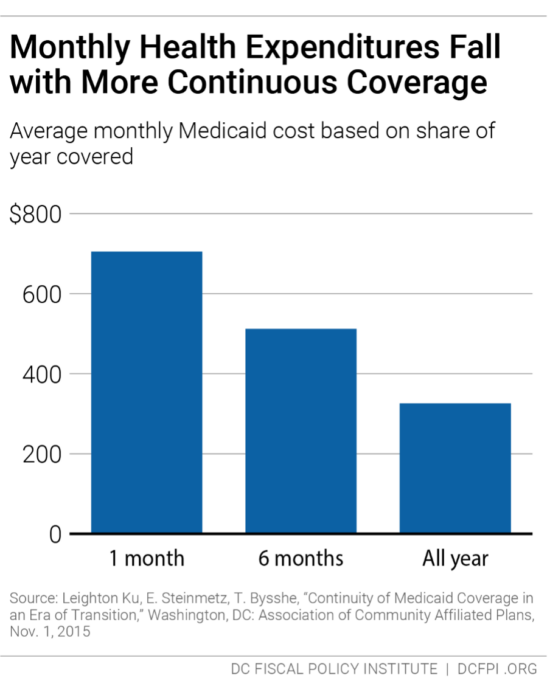
This lack of continuous coverage contributes to poor health outcomes and high costs per person in the Alliance. Churn from frequent recertification increases health program costs because it limits access to preventive care, which means participants often are sicker when they re-enroll, and because sicker residents are most willing to go through the process of maintaining coverage. Healthcare Alliance costs have doubled in the past four years, even though participation has not grown. The cost increases appear to reflect other factors, including a growing number of older participants.[15]
The six-month recertification requirement also creates problems for other residents seeking public benefits. Data collected in 2015 suggest that Alliance recipients make up one-fourth of service center traffic in a given month, even though they represent a very small portion of service center clients.[16]
It is worth noting that DHCF director Turnage and senior staff met several times over the past year with DCFPI and other advocates to discuss this issue, and we appreciate their openness. DHCF staff also engaged in some analysis of Alliance participants, and in my opinion, the research did not point to widespread fraud. This is important given that concern over possible fraud is the primary argument made by DHCF for keeping the current 6-month recertification rule.
- For example, DHCF has concern that some non-residents use a fake DC address to apply for the Alliance, and that in some cases, many people use the same address. But their own analysis found that only 6 percent of Alliance participants are in homes with five or more Alliance participants.[17]
- DHCF also compared participants who cycled on and off with those that cycled off and did not return—with the possibility that some of those who didn’t return may have been on the Alliance fraudulently. But DHCF found the characteristics of those who cycled off permanently to be roughly the same as those who cycled off and on. For example, roughly the same share in both groups had a connection to a non-DC address. The similarity suggests that people who cycle off permanently may be eligible but simply discouraged from remaining on the Alliance by burdensome rules.
Research from Medicaid, for example, shows that average health care costs go down the longer participants have coverage (Figure 2). DCFPI recommends the agency look at recipients who normally would have cycled off the Alliance but did not because of the waiver of the recertification requirement during the public health crisis to see how the longer coverage affected their health and health care costs.
DC has been a leader in expanding health insurance coverage to improve resident health and reduce health disparities. Eliminating barriers to care is a critical component of those important city goals and would go a long way towards affirming support for our immigrant neighbors. This is particularly important now as DC Latinx residents have a higher incidence of coronavirus infection per capita than Blacks and whites, at 10,980 per 100,000 people compared to 6,151 and 3,670 per 100,000 people respectively.[18] These residents need health insurance so they can receive the care they need.
Thank you for the chance to submit this testimony.
[1] “Traumatic Brain Injury & Concussion,” Center for Disease Control and Prevention, http://www.cdc.gov/traumaticbraininjury/
[2] Suzanne Polinder, Juanita A. Haagsma, David van Klaveren, Ewout W. Steyerberg, and Ed F. van Beeck, “Health-Related Quality of Life after TBI: A Systematic Review of Study Design, Instruments, Measurement Properties, and Outcome,” Population Health Metrics (February 17, 2015), https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4342191/
[3] Jennifer L. Highley and Brenda J. Proffit, Traumatic Brain Injury Among Homeless Persons: Etiology, prevalence, and severity, Health Care for the Homeless Clinicians’ Network, revised June 2008, http://www.nhchc.org/wpcontent/uploads/2011/12/TBIAmongHomelessPersons_2008.pdf.
[4] Jane Topolovec-Vranic, Naomi Ennis, Angela Colantonio, Michael D. Cusimano, Stephen W. Hwang, Pia Kontos, Donna Oucherlony, and Vicky Stergiopoulos, “Traumatic brain injury among people who are homeless: a systematic review,” BMC Public Health, 2012, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3538158/pdf/1471-2458-12-1059.pdf
[5] “Findings from the District of Columbia Traumatic Brain Injury Needs and Resources Assessment of Homeless Adult Individuals, Homeless Shelter Providers, TBI Survivors and Family Focus Group, TBI Service Agency/Organizations,” DC Department of Health, revised August 2010, http ://www.nchv.org/images/uploads/DC_TBI_Report.pdf
[6] Ibid.
[7] Amy Burkowski, David Freeman, Faiza Majeed, Jennifer “Niki” Novak, Paul Rubenstein, and Celeste Valente, “Traumatic Brain Injury in the District: The Ignored Injury: A Paper Examining the Prevalence of TBI in the District and the Need for Services,” revised July 2018, http://www.uls-dc.org/media/1150/tbi-white-paper-final-7-25-18.pdf
[8] “Findings from the District of Columbia Traumatic Brain Injury Needs and Resources Assessment”
[9] Ibid
[10] Ibid.
[11] Amy Burkowski, David Freeman, Faiza Majeed, Jennifer “Niki” Novak, Paul Rubenstein, and Celeste Valente
[12] Ed Lazere, “No Way to Run a Healthcare Program: DC’s Access Barriers for Immigrants Contribute to Poor Outcomes and Higher Costs,” DC Fiscal Policy Institute, revised March 17, 2019, https://www.dcfpi.org/all/no-way-to-run-a-healthcare-program-dcs-access-barriers-for-immigrants-contribute-to-poor-outcomes-and-higher-costs/
[13] “Uninsured Rates for the Nonelderly by Race/Ethnicity,” Kaiser Family Foundation, 2019, https://www.kff.org/uninsured/state-indicator/nonelderly-uninsured-rate-by-raceethnicity/?dataView=0¤tTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D
[14] Ed Lazere
[15] Ibid
[16] Wes Rivers, DC Fiscal Policy Institute, and Chelsea Sharon, Legal Aid Society of the District of Columbia, “Testimony for Public Oversight Hearing on the Performance of the Economic Security Administration of the Department of Human Services District of Columbia Council Committee on Health and Human Services,” revised March 12, 2015, https://www.legalaiddc.org/wp-content/uploads/2015/03/CSharon3.12.15.pdf
[17] Department of Health Care Finance information provided to DCFPI and partners.
[18] “The Covid Tracking Project,” The Atlantic, last updated March 2, 2021, https://covidtracking.com/data/state/district-of-columbia
