Chairman Gray and other members of the Council, thank you for the opportunity to testify today. My name is Ed Lazere, and I am the Executive Director of the DC Fiscal Policy Institute. DCFPI is a non-profit organization that promotes budget choices to address DC’s economic and racial inequities and to build widespread prosperity in the District of Columbia, through independent research and policy recommendations.
I am here today to encourage the Council to use the FY 2020 budget to strengthen the DC Healthcare Alliance, a program that provides critical health care coverage to residents with low-incomes who do not qualify for Medicaid, most of whom are immigrants. DCFPI urges the Council to fund the D.C. Healthcare Alliance Re-Enrollment Reform Amendment Act of 2017, which would eliminate barriers to accessing the Alliance that DC imposes. These barriers are both harming the health of immigrants and undermining the program. The legislation would replace an onerous requirement to show up in person every six months to maintain benefits with annual re-certification and allowing participants to renew their eligibility at community health providers. Implementing this legislation would improve the health of DC residents and help stabilize the Alliance.
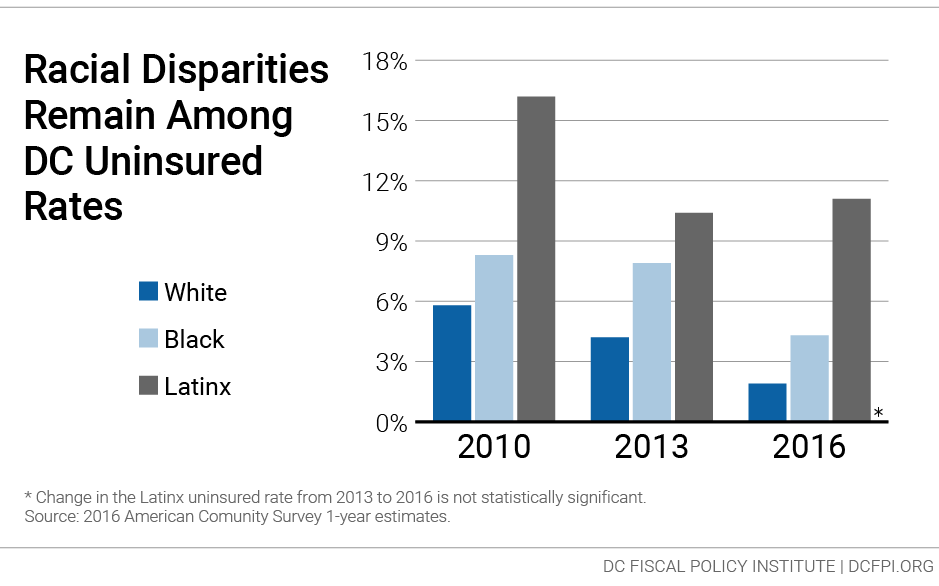
The Alliance is a critical source of health care coverage for DC’s immigrants and a key part of DC’s effort to support universal health insurance coverage. It’s important to remember that the uninsured rate among Latinx residents in DC is far higher than for any other racial or ethnic group. The Alliance is a relatively small program, with an average of about 15,000 residents, which makes it vulnerable. Health problems among a small share of members are hard to spread when the pool is small, and small changes in the makeup of that pool to be less healthy can have a big effect. That makes it important for the Alliance to have a stable and diverse pool.
Yet as outlined in a recent policy brief from DCFPI, the six-month in-person recertification requirement is undermining the Alliance, contributing to poor health outcomes and unnecessarily high program costs.[1] The Alliance suffers from a very high rate of turnover, or “churn.” Over the past 18 months, only 55 percent of Alliance participants renewed their eligibility when it came up, according to data from the Department of Health Care Finance. This means that many Alliance participants have only intermittent health coverage.
The reason for this high rate of churn is not a mystery. Research and common sense confirm that short recertification periods lead to a high rate of churn. Given that many Alliance members are working at jobs without paid leave and that visiting a social service center can take an entire day or longer, it’s not surprising that many do not renew their benefits. Imagine having to visit the DMV in person every six months to keep a driver’s license.
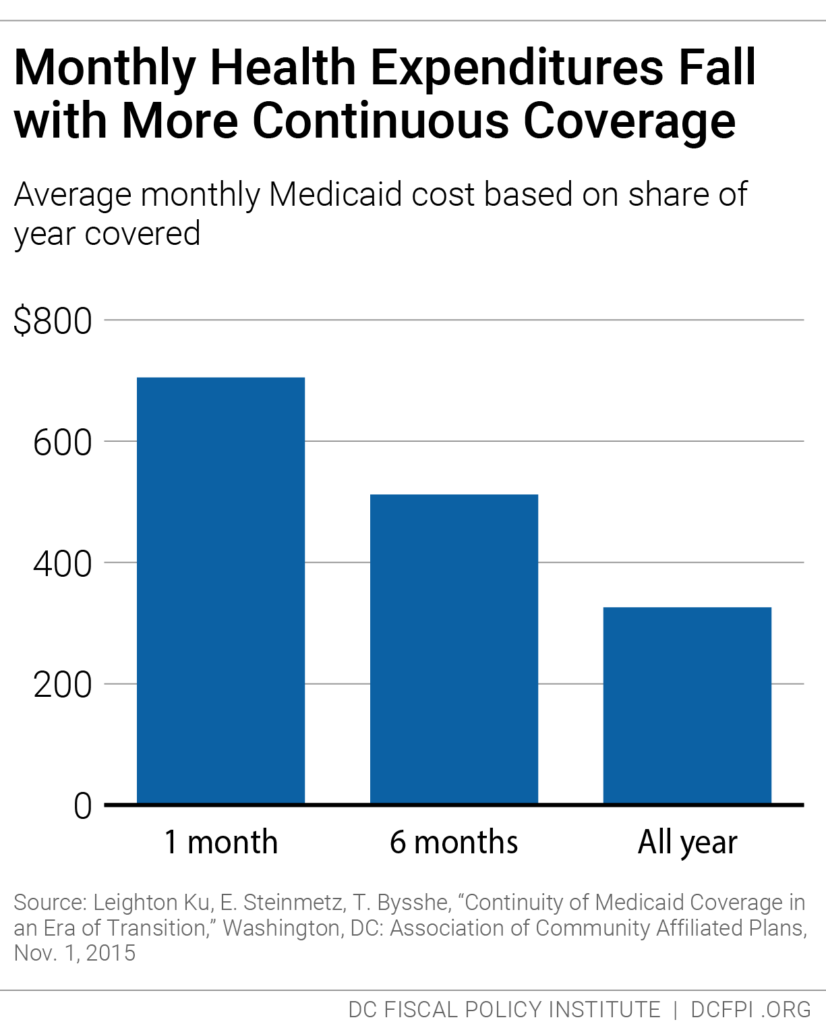
Churn from frequent recertification increases health program costs because it limits access to preventive care, which means participants often are sicker when they re-enroll, and because sicker residents are most willing to go through the process of maintaining coverage. The Healthcare Alliance costs have doubled in the past four years, even though participation has not grown, and the budget for FY 2020 reflects another substantial increase.
DCFPI appreciates the District’s ongoing commitment to the Alliance. We urge the Mayor and Council to explore the many factors behind its rising costs, which includes an increasing number of older participants and greater use of expensive hospitalization services.
But we also urge the Council to take immediate steps in the FY 2020 budget to replace the six-month in-person recertification barrier, the one factor that is directly in our control and that we know would strengthen the Alliance and help stabilize its costs. This would improve health outcomes for DC’s immigrants and reduce monthly per-person program costs as residents receive better care and as healthier residents, currently discouraged from staying on, are able to maintain coverage. Research from Medicaid, for example, shows that average monthly health care costs go down the longer participants have coverage.
Replacing the current re-certification process also would help address another problem: long lines at DC’s ESA social service intake centers. Because Alliance members must certify more often than participants in other programs, they represent a large share of people visiting ESA centers. The long lines and other difficulties applying for benefits affects not only Alliance participants but all residents seeking assistance at an ESA center. Moving to annual re-certification in the Alliance, and enabling recertification through community-based providers, would ease the long lines and daily pressures at ESA centers.
Thank you for the chance to testify.
[1] Ed Lazere, DC Fiscal Policy Institute, “No Way to Run a Health Care Program: DC’s Access Barriers for Immigrants Contribute to Poor Outcomes and Higher Costs,” March 17, 2019.