The District should do more to connect residents on Medicaid with basic health services, which would improve their health and reduce District costs by avoiding costly emergency services. That conclusion is based on a recent report on three managed care organizations (MCOs) that have served 175,000 DC Medicaid participants for a year, but have not improved access to health services or coordination of patient care. Better oversight of this program, including more information on the care they provide, could help to improve access, contain health care costs and improve overall health for DC residents.
 Most DC Medicaid recipients are assigned to one of three MCOs. The District pays each MCO a fee for each enrollee and in return the company reimburses doctors and hospitals for health care services used. An annual review of the MCO program, from the DC Department of Health Care Finance, suggests that the three managed care organizations have struggled to manage patient’s care and as a result, failed to keep costs down.
Most DC Medicaid recipients are assigned to one of three MCOs. The District pays each MCO a fee for each enrollee and in return the company reimburses doctors and hospitals for health care services used. An annual review of the MCO program, from the DC Department of Health Care Finance, suggests that the three managed care organizations have struggled to manage patient’s care and as a result, failed to keep costs down.
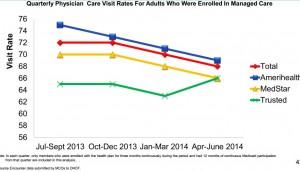
- Only two-thirds of participants regularly visit with a primary care doctor. Seeing a primary care doctor regularly is important to managing health needs, which reduces the use of more costly and intensive services.
- Over three-fifths of emergency room visits by DC Medicaid recipients are for basic care, and a large portion could have been avoided.
- One in twelve hospital visits result in a readmission, some of which could be avoided through better service delivery and follow-up care.
- No MCO provides case management — services for people with higher health needs and chronic health conditions like asthma — to more than 5 percent of members. Case management helps patients get appropriate referrals and follow-up care after seeing a doctor. Given the range of conditions that MCO’s must offer case management services for — including HIV, asthma, mental illness, substance abuse, diabetes, and cardiovascular disease — MCOs should be doing more to identify patients and connect them with services.
Over-reliance on the emergency room and high rates of hospital readmissions cost the MCOs more than $34 million in this first year — which means the MCOs will charge the District more next year.
DCFPI’s transition document for health care details how DC can establish stronger oversight of the Medicaid managed care program. One of the major steps is to collect more data and establish performance benchmarks. Setting standards for things like avoidable emergency room visits can help the city create a payment structure and financial incentives that will lead to better outcomes. The District has already begun this process by collecting the data for the quarterly report, but now that a year has passed, it is time to refine the data and create benchmarks. DCHCF should also allow the public to comment and contribute to the formulation of further data collection and performance standards.
To print a copy of today’s blog, click here.
