The Affordable Care Act has allowed the District to improve access to health care through Medicaid, by making more residents eligible and by expanding Medicaid services. The ACA also changed the way many residents will apply for and renew their benefits starting this fall, in ways that should make it easier to get and keep health coverage. But the changes — particularly in how income is counted to determine Medicaid eligibility — may be confusing to some.
We want to explain those changes today, doing our part to make the transition easier.
Changes in How Medicaid Will Count Income to Determine Eligibility
The Affordable Care Act changed the way DC and the states collect income information from people applying for Medicaid, with the new format closely following how we report income on federal income tax forms. The new method is known as Modified Adjusted Gross Income (MAGI).
This makes sense because the same income rules and application are used to determine whether residents are eligible for tax credits and subsidies to help pay for health plans sold on DC Health Link. The tax credits and subsidies are for people with incomes that are moderate but too high to qualify for Medicaid.
This means that residents who are not sure whether they are eligible for Medicaid or for the tax credits can apply for both using just one application. The new process will also make it easier for administrators to verify income and eligibility through federal data sources.
How to Apply for and Renew Medicaid Benefits
The creation of the DC Health Link — DC’s online, health insurance marketplace — and the new income-counting methods make it easy for DC residents to apply for Medicaid. And they should make it easier to renew their eligibility each year.
Starting in November 2014, the District will send current Medicaid recipients a pre-populated renewal form to collect missing tax and income information. After filling out the form this one time, the renewal process for every year going forward is “passive” — meaning that residents may not have to do anything to maintain their eligibility. The District will match information provided on the form to federal and local data hubs to verify eligibility. The recipient will not have to complete renewal forms again unless the data hubs return inconclusive results.
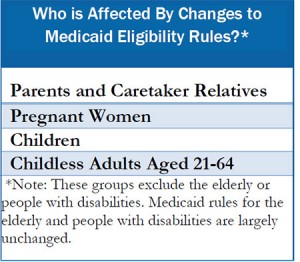
It should be noted that the application and renewal processes remain largely unchanged for people who are Medicaid-eligible due to age or disability status. Moreover, new Medicaid applicants who have applied since October 2013 will not have to fill out the renewal form.
Any time systems change, there are technical glitches and consumer confusion, so providers and consumer representatives should familiarize themselves with the new processes before November. This presentation is a good resource that walks through the renewal form.
To print a copy of today’s blog, click here.