The District has been a leader in using the Affordable Care Act (ACA) to expand health insurance to nearly all of its residents. But we should not stop there. The next step is to focus on providing services to address DC’s long-standing health disparities, including those caused by tobacco use. The District has taken advantage of some — but not all — of the ACA options to enhance tobacco treatment. The District’s next wave in health reform should include aggressively attacking tobacco use in the city.
About one in five District adults smoke, including nearly one in three African-American adults. Residents east of the river are more likely than others to be frequent smokers. This means that tobacco use worsens health disparities across the city.
The District has already taken advantage of two Affordable Care Act provisions to provide tobacco prevention and cessation services, especially among residents who are Medicaid eligible.
- Banning private health insurers from charging tobacco users more for their health plan. The ACA allows DC and the states to ban private insurers from charging smokers more than non-smokers for their health insurance premiums. DC chose to ban rate hikes for tobacco users, as the price increases could prevent lower income residents from accessing the care they need to quit.
- Expanding Medicaid coverage to include face-to-face tobacco counseling and cessation medication for pregnant women. Tobacco use during pregnancy can have serious health effects on the fetus, so the ACA mandated coverage of counseling and cessation drugs for this population. The District amended its Medicaid State Plan this year to include these services.
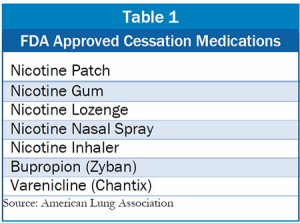 But the District is not doing enough to provide Medicaid coverage for FDA-approved cessation drugs or to cover tobacco counseling services. The ACA requires state Medicaid programs to cover all seven FDA approved cessation drugs (See Table 1) for all enrollees by January 2014. DC covers only three of these drugs (nicotine gum, patch, and lozenge), which means the city is out of compliance with ACA and missing the opportunity to greatly curb preventable disease.
But the District is not doing enough to provide Medicaid coverage for FDA-approved cessation drugs or to cover tobacco counseling services. The ACA requires state Medicaid programs to cover all seven FDA approved cessation drugs (See Table 1) for all enrollees by January 2014. DC covers only three of these drugs (nicotine gum, patch, and lozenge), which means the city is out of compliance with ACA and missing the opportunity to greatly curb preventable disease.
The District also has the option to fund the “tobacco quit-line” — its telephone counseling service — using Medicaid dollars. The District would need to conform the quit-line with proven practices, which could lead to a more effective program and a sustainable funding stream via Medicaid.
Improving health outcomes is not only good for tobacco users and their family and friends. It also will reap long-term healthcare cost savings. A good example is Massachusetts — which implemented comprehensive Medicaid coverage for tobacco cessation services and medication and found that every dollar invested in the cessation program resulted in $3.12 in medical savings.
To print a copy of today’s blog, click here.
